Understanding the Rotator Cuff Healing Index (RoHI)
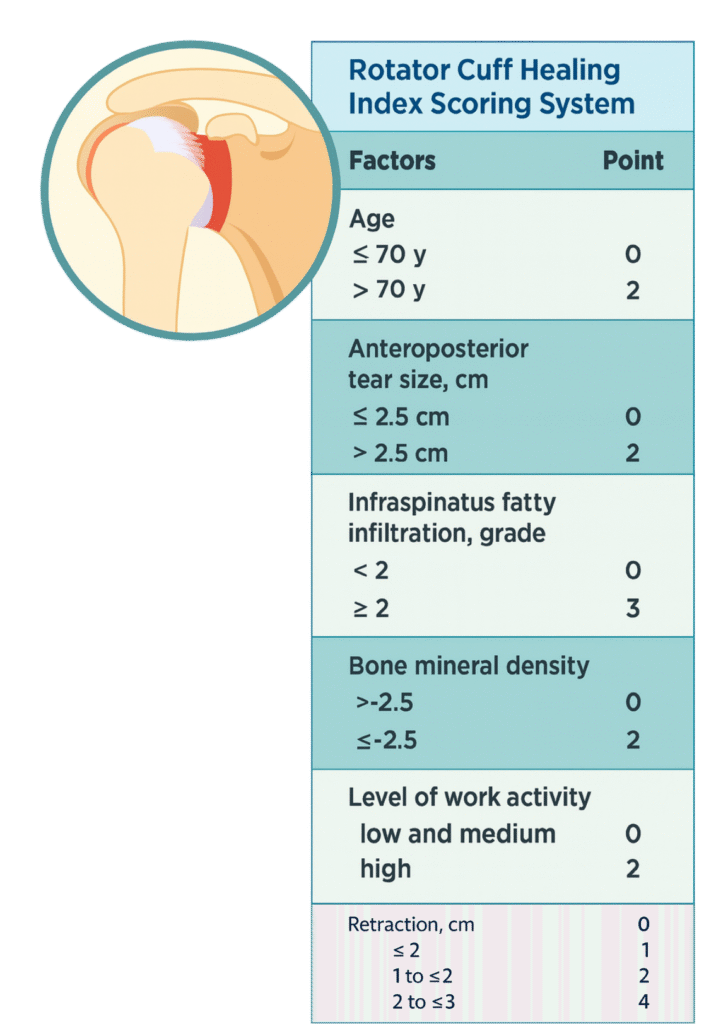
Rotator cuff repair remains one of the most performed yet unpredictable procedures in orthopedics. Despite surgical advances, retear rates still range widely, from under 20% to over 50% depending on patient factors. To better anticipate outcomes, Kwon et al. (2019) developed the Rotator Cuff Healing Index (RoHI): a 15-point scoring system designed to quantify healing risk after surgical repair.
What Goes into a RoHI Score?
The RoHI integrates 6 variables commonly linked to rotator cuff healing outcomes:
- Patient Age (2 points if >70)
- Tear Size (AP dimension) (>2.5 cm = 2 points)
- Tear Retraction (up to 4 points)
- Infraspinatus Fatty Infiltration (Goutallier ≥2 = 3 points)
- Bone Mineral Density (T-score ≤–2.5 = 2 points)
- Level of Work Activity (high = 2 points)
A cumulative RoHI score helps surgeons estimate a patient’s likelihood of healing. In the original cohort, patients with a RoHI of 4 or less had a 94% healing rate; those scoring 10 or higher had only a 14% chance of healing post-repair.
Applying RoHI in Surgical Planning
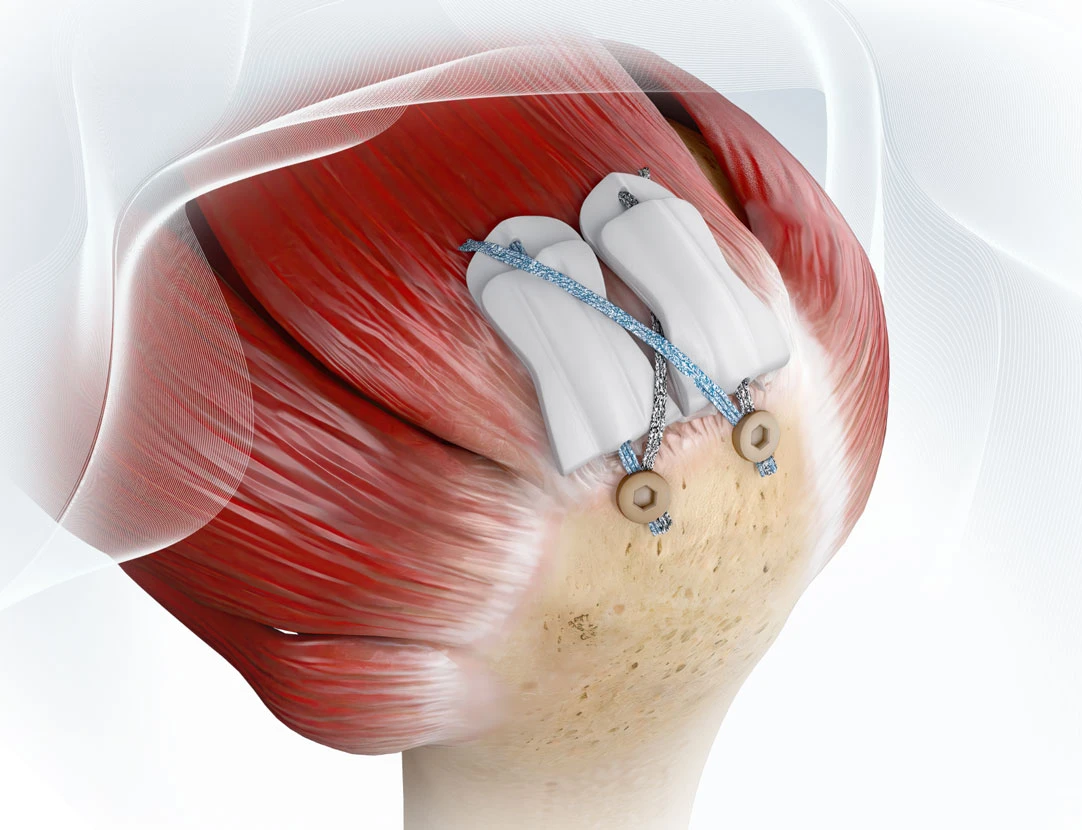
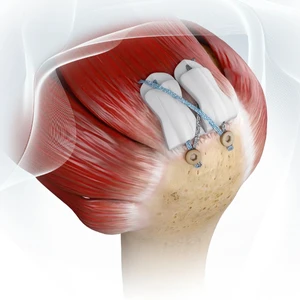
While RoHI doesn’t replace clinical judgment, it provides a valuable risk stratification tool. A patient with a score ≥7 may warrant additional consideration, such as graft augmentation strategies. Emerging evidence suggests that tissue scaffolds, including interpositional and onlay implants, can support healing at the tendon-bone interface and suture-tendon interface in these cases.
Why Healing Support Matters
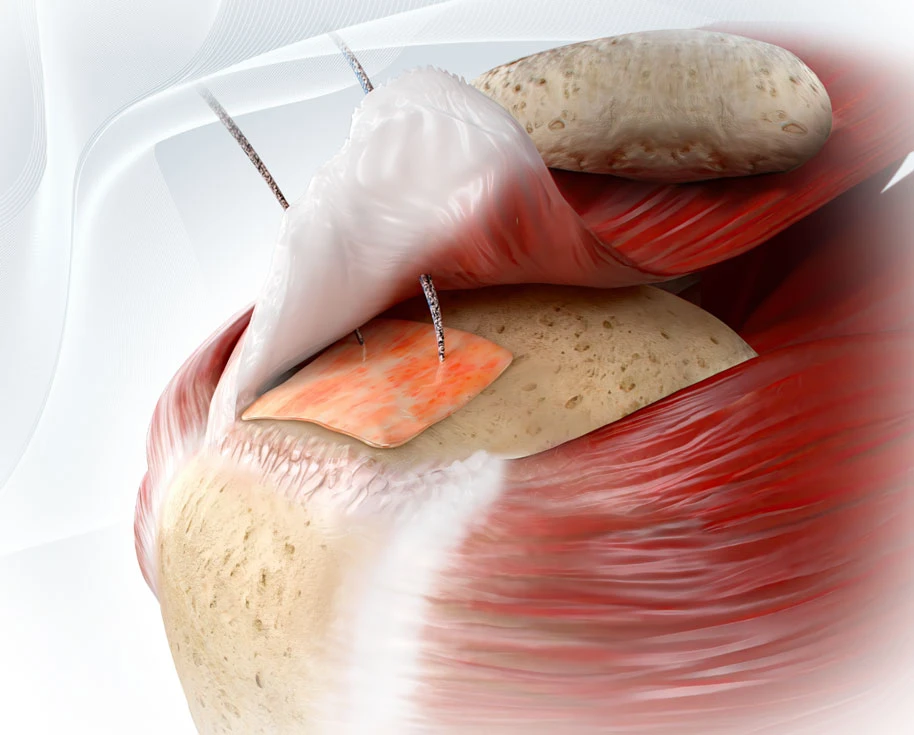
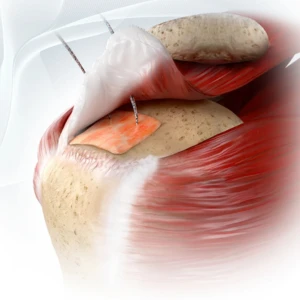
Failure of tendon healing often occurs at the suture-tendon junction or the tendon-bone interface, also known as the enthesis. For patients flagged by RoHI as high-risk, enhancing the healing environment could help reduce retear likelihood. While no product can guarantee a successful outcome, ROTIUM® Bioresorbable Wick is designed to retain the patient’s own biology at the repair site and support a favorable biologic environment, which may help address biologic deficiencies that traditional mechanical fixation cannot.
Atreon’s newest technology, BioCharge® Autobiologic Matrix, is engineered to reinforce the tendon-suture interface, a known point of failure in high-risk repairs. Its placement on the bursal side supports cellular activity and tissue organization, helping deter suture cut-through and complementing biologic support at both ends of the healing challenge. This uniquely designed device has a built-in delivery system that makes implantation very efficient in the OR.
Key Takeaway for Surgeons
RoHI is a practical, evidence-based tool for anticipating healing outcomes and tailoring interventions accordingly. While RoHI still needs further validation through prospective studies, integrating it into preoperative planning enables more personalized, data-informed care and may help guide decisions on when to consider biologic augmentation strategies.
References
- Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The Rotator Cuff Healing Index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019;47(1):173-180. doi:10.1177/0363546518810763
- Jackson GR, Bedi A, Denard PJ. Graft augmentation of repairable rotator cuff tears: an algorithmic approach based on healing rates. Arthroscopy. 2022;38(7):2342-2347. doi:10.1016/j.arthro.2021.10.032
- Manop K, et al. Risk factors for rotator cuff repair failure and reliability of the Rotator Cuff Healing Index (RoHI) in a Thai population. 2023.
- Korean Orthopedic Association Poster PP068. Modified Rotator Cuff Healing Index (mRoHI): Simplifying prediction of rotator cuff healing outcomes. KOA 2024.
- Kim D, et al. Predictive Healing Score for Decision Making in Rotator Cuff Repair. 2024.
- Denard PJ, et al. Augmentation techniques for rotator cuff repairs: Current evidence and future directions. 2021.