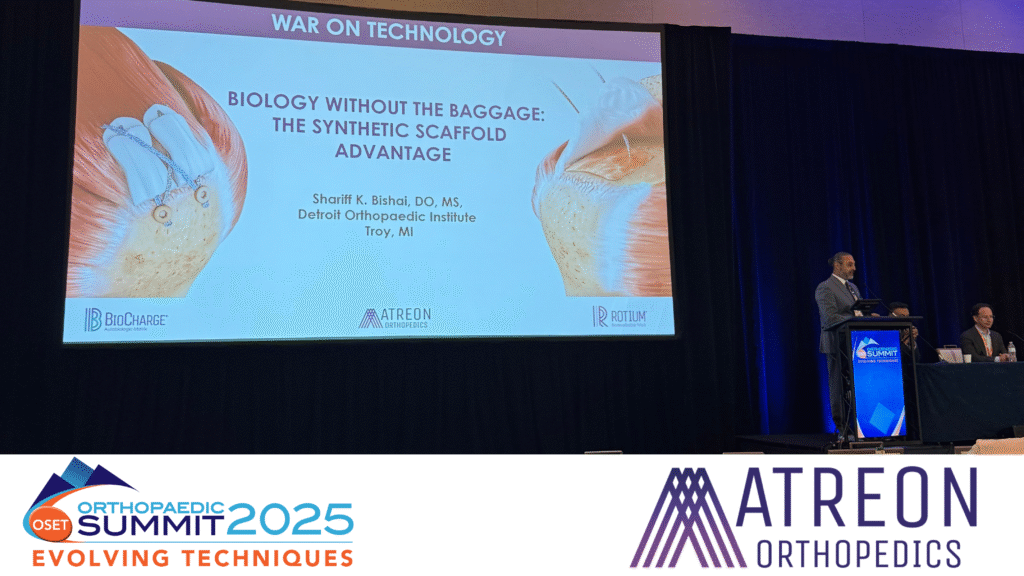
Synthetic Scaffold Advantage in Rotator Cuff Repair, Featuring Dr. Shariff K. Bishai at OSET 2025
Why Synthetic Scaffolds Are Gaining Ground in Shoulder Surgery
At the 2025 Orthopedic Summit (OSET) in Las Vegas, Dr. Shariff K. Bishai delivered a compelling presentation titled “Biology Without the Baggage: The Synthetic Scaffold Advantage.” As part of the conference’s “War on Technology” track, his talk spotlighted the evolving conversation around biologic augmentation in rotator cuff repair, particularly the role of synthetic scaffolds as an emerging option. Many in the field see biologic augmentation as a promising approach to address the underlying healing deficiencies that persist when repairs fail.
Data from a 600+ patient cohort highlights how variables like tear size, age, tissue quality, and revision status can drastically increase the risk of retear. For “at-risk” patients—those scoring 4–10 on the ROHI scale, enhancing the healing environment at the enthesis may support improved healing outcomes in appropriate patients, based on early clinical data (Kwon, 2018).
Limitations of Dermal Allograft Augmentation
Dermal patches have long been used in augmentation of massive or revision rotator cuff repairs. While intended to provide structural support and reduce tension at the repair site, these grafts come with challenges:
- High cost
- Added surgical time and complexity
- Variability in biologic response
- Risk of inconsistent integration
According to a recent publication, 70 months after implantation, the dermal allograft used in SCR failed to remodel into normal tendinous tissue, showing persistent acellularity and randomly oriented collagen rather than tendon-like structure (Best, 2025). These factors can contribute to unpredictable outcomes, especially in procedures where consistency and efficiency are critical.
The Tradeoffs of Collagen-Based Patches
Collagen-based patches, often derived from bovine collagen, offer a biologic approach designed to stimulate healing through native signaling cues. However, concerns persist around:
- Inflammatory responses due to xenogenic proteins
- Lack of mechanical strength during early healing
- Irregular degradation and remodeling timelines
Multiple published studies have shown that in some cases, collagen-based bioinductive implants may not outperform standard repairs, prompting a closer look at their value in everyday surgical practice. One such study concluded, “At minimum 2-year follow-up, patients undergoing primary arthroscopic rotator cuff repair with bovine collagen implant augmentation had a greater proportion of reoperation due to inflammation and stiffness compared with patients who did not receive the implant.” (S, Umasuthan, 2025). Lippincott Journals
A New Option: Synthetic Scaffolds with Purpose-Built Design
Autobiologic vs. Bioinductive Healing
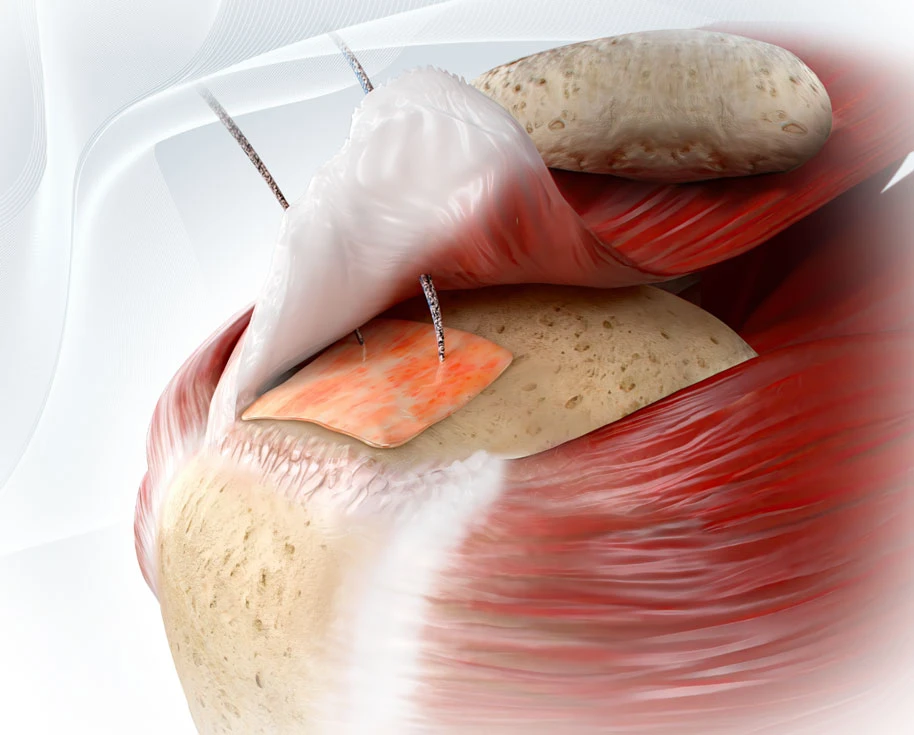
Synthetic scaffolds like ROTIUM represent a new class of technology: autobiologic implants. Unlike bioinductive materials that introduce foreign biologic components (e.g., bovine collagen) to stimulate healing, autobiologic scaffolds work by leveraging the patient’s own healing factors—blood, cells, and cytokines—delivered directly to the tendon-bone interface or repair site. These implants do not carry donor or animal tissue but instead serve as a biologically inert conduit that promotes natural, localized tissue remodeling.
Synthetic scaffolds represent a different strategy: replicating the mechanical and biologic support of the native extracellular matrix using engineered, fully resorbable materials. Benefits of this approach include:
- Predictable resorption profiles (over 3-6 months)
- Reproducible quality and performance
- No risk of immune rejection
- Integration into standard techniques without added surgical time
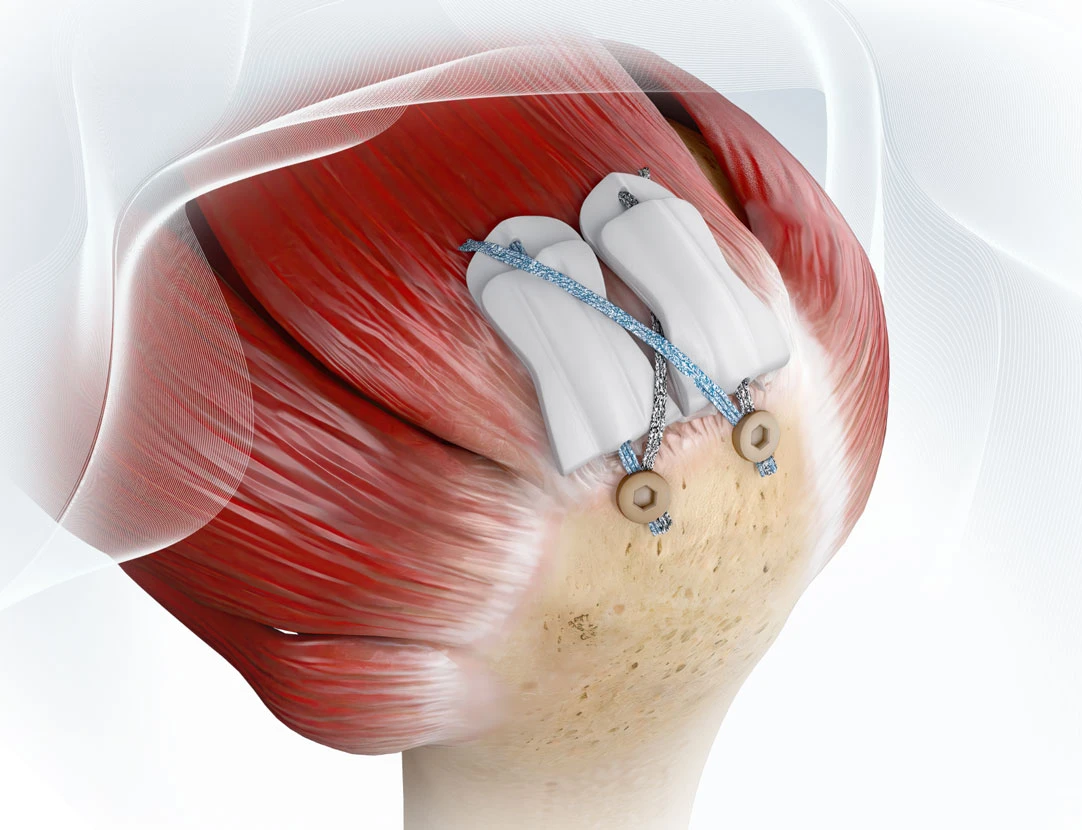
One such product is the ROTIUM® Bioresorbable Wick, an interpositional scaffold FDA-cleared for use in tendon repair, including rotator cuff augmentation. It’s a “biologic delivery device” for autologous healing factors directly at the tendon-bone interface, without requiring additional instrumentation or cumbersome delivery systems.
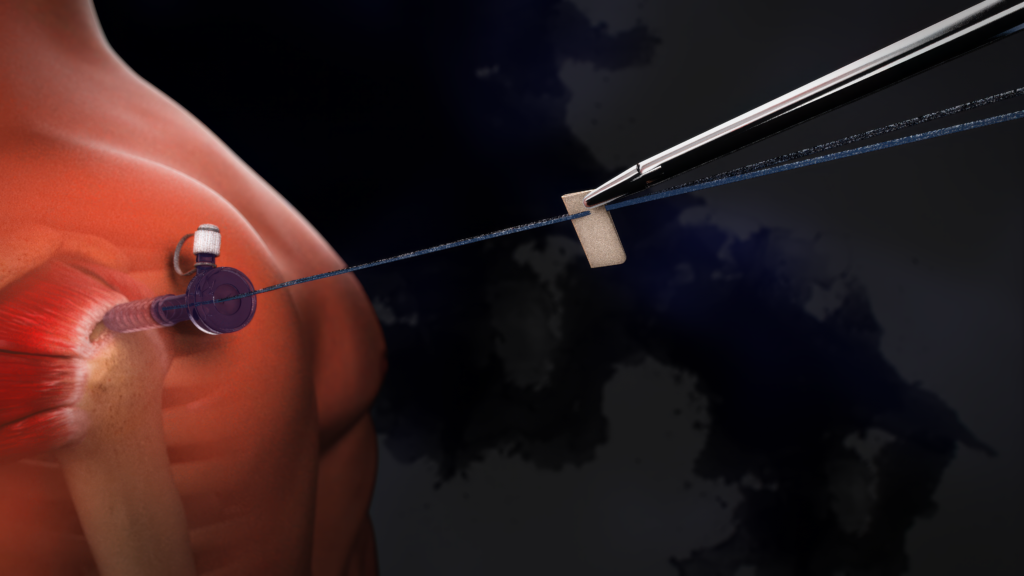
Versatility Across All Tendon Repairs
ROTIUM is FDA-cleared for use across a wide range of tendon repairs – not just in the shoulder – and can be placed at the tendon-bone interface in procedures involving the elbow, hip, knee, foot, and ankle. BioCharge is designed specifically for rotator cuff repair, where it uses a built-in suture tunnel that acts as a delivery mechanism.
ROTIUM and BioCharge have been used in over 16,000 procedures to date (reflects accumulated usage, not clinical study volume).
Clinical Implications and Takeaways
In summary, synthetic scaffold technology offers surgeons a biologically active solution that’s reproducible, cost-effective, and simple to deploy, a valuable asset in both hospital and ASC settings.
Learn More
Explore Atreon’s ROTIUM Bioresorbable Wick or visit our Technology Overview to see how our scaffold platform is helping reshape tendon repair.
External Links:
References
- Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The Rotator Cuff Healing Index: A New Scoring System to Predict Rotator Cuff Healing After Surgical Repair. The American Journal of Sports Medicine. 2018;47(1):173-180. doi:10.1177/0363546518810763
- Failure of dermal allograft remodeling and integration after superior capsular reconstruction for an irreparable rotator cuff tear: a case study 70 months postimplantation. Best, J, S Arnoczky, DVMb, SK. Bishai, DO, et al. JSES International, Volume 9, Issue 4, 1159 – 1163. 2025.9(4): 1159-1163
- Haft M, Li SS, Pearson ZC, Ahiarakwe U, Bettencourt AF, Srikumaran U. No short-term clinical benefit to bovine collagen implant augmentation in primary rotator cuff repair: a matched retrospective study. Clin Orthop Relat Res. 2025;483(3):442-452.